Introduction
Welcome to Basavatarakam Indo American Cancer Hospital and Research Institute, where we are committed to providing comprehensive information about cancer to empower you in your journey toward better health. In this detailed guide, we will explore the various facets of breast cancer in a way that is easy to understand for everyone.
![]()
Section 1: What is Breast Cancer?
Breast cancer is a disease that originates in the cells of the breast. It is not exclusive to any gender; both women and, though less frequently, men can be affected. Breast cancer occurs when normal breast cells transform and grow uncontrollably, forming a lump or tumor. These tumors can be benign (non-cancerous) or malignant (cancerous).

Section 2: Understanding Breast Anatomy
To understand breast cancer fully, it’s important to grasp the basic anatomy of the female breast. The breast consists of three primary components: lobules, ducts, and connective tissue.
-
Lobules: These are glands responsible for producing milk.
-
Ducts: Tubes that transport milk to the nipple.
-
Connective Tissue: Comprising fibrous and fatty tissue, which surrounds and protects the glands and ducts.
Breast cancer can develop in any of these three components, but it most commonly starts in the ducts, which is why the term “ductal carcinoma” is often used.
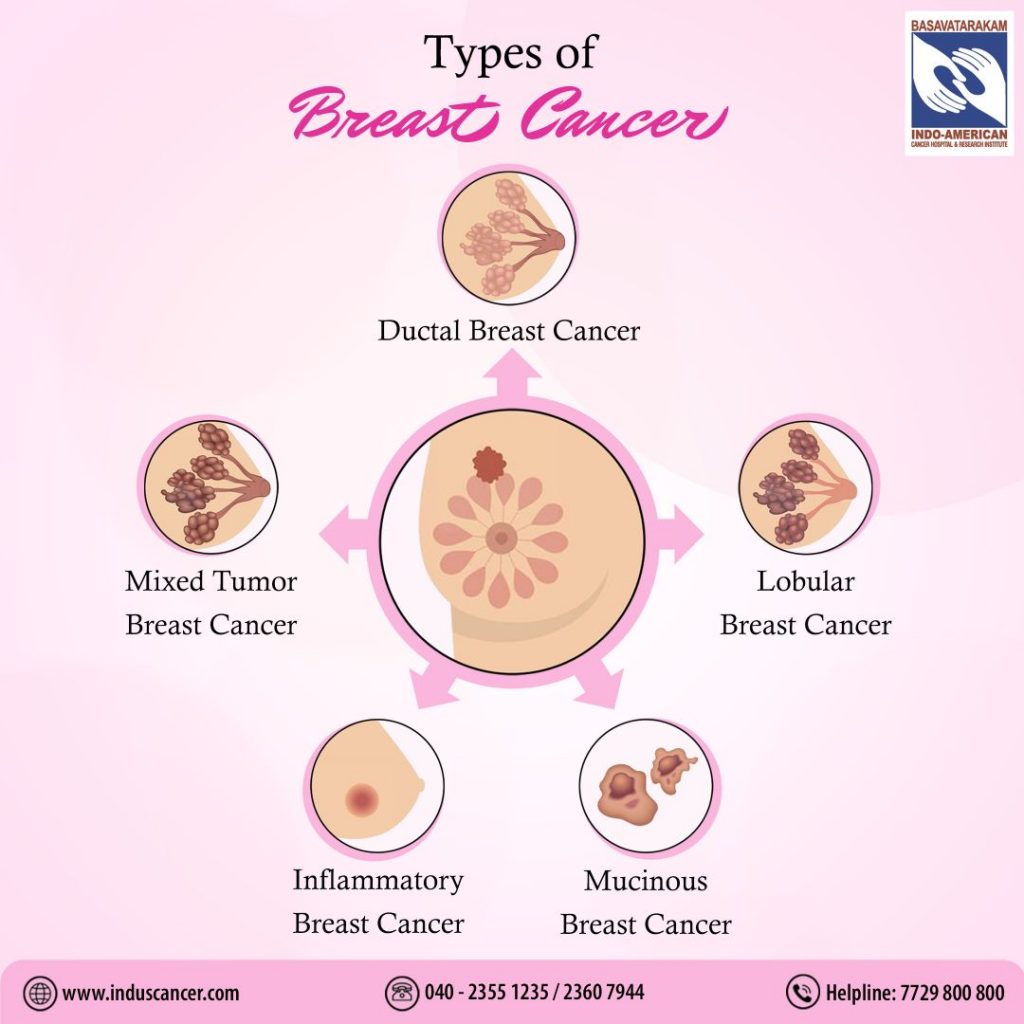
Section 3: Types of Breast Cancer
Breast cancer isn’t a singular disease; it encompasses a group of diseases. The two most prevalent types are:
-
Ductal Carcinoma In Situ (DCIS): This is a non-invasive cancer where abnormal cells are found in the lining of a breast duct but have not spread outside the duct.
-
Invasive Ductal Carcinoma (IDC): This is the most common type of breast cancer, characterized by cancer cells that have invaded the surrounding breast tissues.
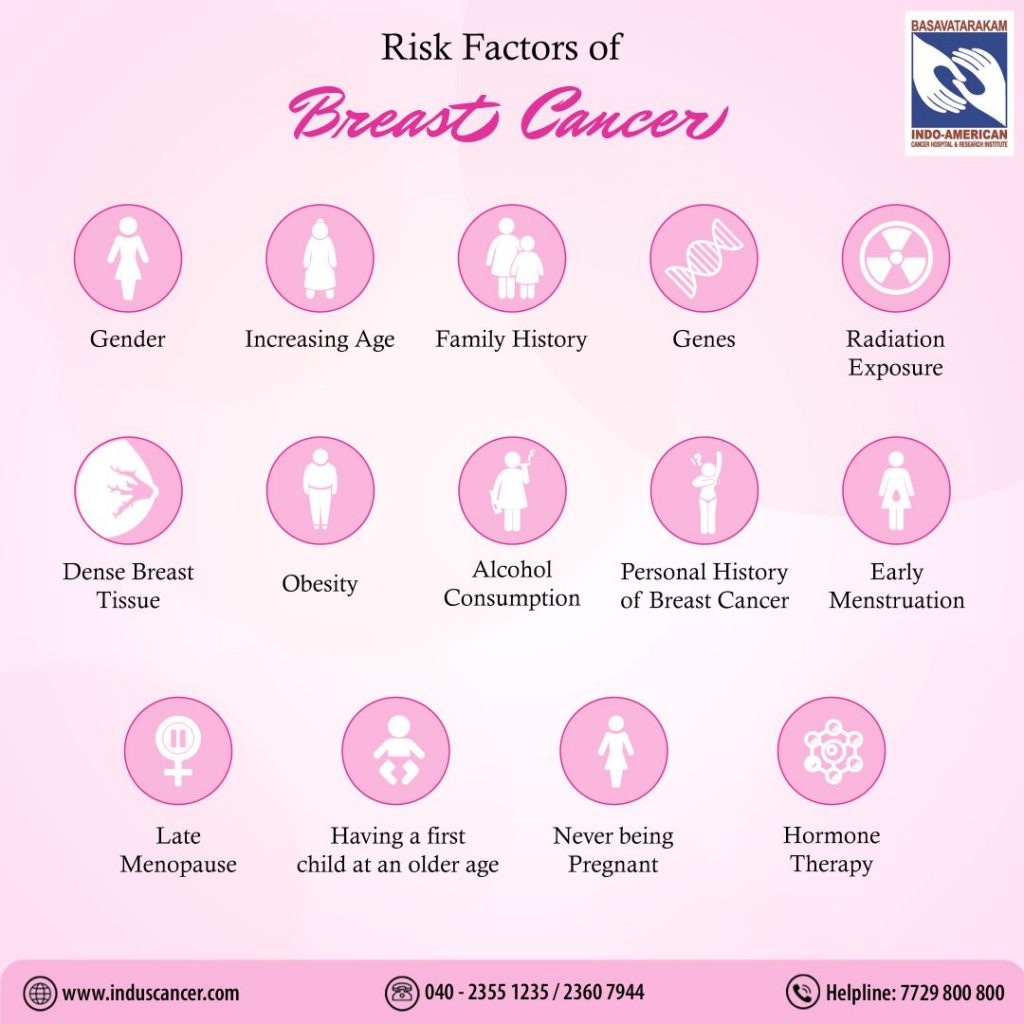
Section 4: Risk Factors
Understanding the risk factors for breast cancer is crucial for proactive health management. While some risk factors, such as age and gender, are beyond our control, others can be managed. Common risk factors include:
-
Age: The risk of breast cancer increases with age.
-
Gender: Breast cancer is more common in women, but men can also develop it.
-
Family History: A family history of breast cancer can increase your risk.
-
Genetics: Inherited gene mutations (BRCA1 and BRCA2) can predispose individuals to breast cancer.
-
Hormone Replacement Therapy (HRT): Long-term use of HRT may increase the risk.
-
Lifestyle Factors: This includes factors like alcohol consumption, obesity, and physical inactivity.
Section 5: Signs and Symptoms
Recognizing the signs and symptoms of breast cancer is crucial for early detection. These may include:
-
Breast Lumps: These are often painless but should be evaluated.
-
Changes in Breast Size or Shape: One breast becoming larger or lower than the other.
-
Nipple Changes: Inversion, discharge, or new pain.
-
Skin Changes: Dimpling or redness of the breast skin.

Section 6: Diagnosis and Staging
Breast cancer diagnosis usually involves a combination of:
1. Clinical Examination 2. Imaging (Mammogram, MRI, Ultrsound Etc..) 3. Biopsy.
-
Mammography: An X-ray of the breast to detect abnormalities.
-
MRI or Ultrasound: These can provide additional information.
-
Biopsy: The removal of a small tissue sample for examination.
Once diagnosed, the cancer is staged, which helps determine its extent and guide treatment decisions.
Section 7: Treatment Options
The good news is that many breast cancers are highly treatable. Treatment options may include:
-
Surgery: Removal of the tumor or, in some cases, the entire breast (mastectomy).
-
Radiation: High-energy X-rays to target and destroy cancer cells.
-
Chemotherapy: Medications to kill or slow down cancer cells.
-
Hormone Therapy: Drugs to block hormones that fuel certain types of breast cancer.
-
Targeted Therapy: Medications that target specific characteristics of cancer cells.
-
Immunotherapy: Treatment that boosts the body’s immune system to fight cancer.
The choice of treatment depends on factors like the cancer’s stage, type, and individual patient considerations.
Section 8: The Importance of Early Detection
Breast cancer, like many cancers, is most treatable when caught early. Regular breast self-exams and routine mammograms are recommended for early detection.
Section 9: Breast Cancer Prevention and Screening
Preventing breast cancer, where possible, is an important part of maintaining good health. While not all risk factors can be controlled, there are steps you can take to reduce your risk and promote early detection.
1. Lifestyle Modifications:
-
Healthy Diet: A diet rich in fruits, vegetables, whole grains, and low in saturated fats can contribute to overall health. Some studies suggest that a diet high in fruits and vegetables may be associated with a lower risk of breast cancer.
-
Physical Activity: Regular physical activity can help maintain a healthy weight, which is associated with a reduced risk of breast cancer.
-
Limit Alcohol Consumption: Excessive alcohol intake is a risk factor for breast cancer. If you choose to drink, do so in moderation.
2. Breastfeeding:
Breastfeeding has been associated with a reduced risk of breast cancer. It’s not only beneficial for your child but also offers potential long-term health benefits for you.
3. Hormone Replacement Therapy (HRT):
If you are considering hormone replacement therapy to manage menopausal symptoms, discuss the risks and benefits with your healthcare provider. Long-term HRT use may be linked to a higher risk of breast cancer.
4. Breast Self-Exams:
Perform regular breast self-exams. Familiarizing yourself with the normal look and feel of your breasts can help you detect any changes. If you notice any unusual lumps, skin changes, or other abnormalities, seek medical attention promptly.
5. Clinical Breast Exams:
Regular clinical breast exams by a healthcare provider are an essential part of breast cancer screening. These exams can help detect changes in your breasts that might not be apparent during self-exams.
6. Mammography:
Regular mammograms are a critical component of breast cancer screening, especially for women over 40. These X-ray images can detect breast cancer in its early stages, often before symptoms appear.
7. Genetic Testing:
For individuals with a strong family history of breast cancer or known genetic mutations, genetic testing and counseling can help assess and manage their risk.
Prevention and early detection go hand in hand in the fight against breast cancer. By adopting a healthy lifestyle and adhering to recommended screening guidelines, you can significantly reduce your risk and increase the chances of early detection, leading to more effective treatment and better outcomes.
For personalized guidance on breast cancer prevention and screening, consult with your healthcare provider. At Basavatarakam Indo American Cancer Hospital and Research Institute, we are here to support your journey to better health.
Conclusion
Knowledge is a powerful tool. If you or someone you know is dealing with breast cancer, it’s important to reach out to healthcare professionals for guidance and support. The field of breast cancer research and treatment is continually advancing, providing hope for those affected by this disease.
Stay informed, stay vigilant, and never underestimate the value of regular check-ups and screenings in the fight against breast cancer.
At Basavatarakam Indo American Cancer Hospital and Research Institute, we are here to support you on your journey to better health.
Some FAQ’s:
1. What is Breast Cancer?
Q: What is breast cancer and how does it develop?
A: Breast cancer occurs when cells in the breast grow uncontrollably, forming a tumor. It often starts in the ducts or lobules of the breast. Early detection increases the chances of successful treatment. Regular screenings and awareness of symptoms can help identify cancer before it spreads.
2. Who is at Risk for Breast Cancer?
Q: What are the risk factors for breast cancer?
A: Breast cancer risk factors are classified into Modifiable and Non-Modifiable. Non-Modifiable factors include being female, aging, family history, and genetic mutations (BRCA1/2). While genetics cannot be altered, adopting a healthy lifestyle and regular screenings can reduce overall risk. Modifiable factors include smoking, late pregnancy, inadequate breastfeeding, obesity, and alcohol consumption, which can be managed to lower risk.
3. Signs and Symptoms of Breast Cancer
Q: What are the most common signs and symptoms of breast cancer?
A: The most common symptom is a lump in the breast or underarm. Other signs include changes in breast shape or size, nipple discharge (especially blood), skin changes, or nipple retraction. Early detection through self-exams and regular screenings can be life-saving.
4. Importance of Early Detection
Q: Why is early detection of breast cancer important?
A: Early detection, particularly through mammograms and self-exams, allows treatment to begin at a stage when cancer is most treatable. The survival rate for localized breast cancer is significantly higher than when it has spread to other parts of the body.
5. Self-Examination: How to Check for Breast Lumps
Q: How can I perform a breast self-exam?
A: Begin by inspecting your breasts in a mirror for visible changes. Use your opposite hand to feel each breast in a circular motion from the outer edges to the nipple. Look for lumps, hard knots, or thickened tissue. Conduct this exam 7-10 days after your menstrual cycle and consult a doctor if anything unusual is detected.
6. Can Men Get Breast Cancer?
Q: Can men develop breast cancer too?
A: Yes, though rare, men can develop breast cancer. Signs include a lump under the nipple, pain, or changes in the breast area. Men with a family history of breast cancer or BRCA mutations are at higher risk and should consult a doctor if they notice symptoms.
7. The Role of Genetics in Breast Cancer
Q: How do genetics impact breast cancer risk?
A: Mutations in BRCA1 and BRCA2 genes significantly increase the risk of breast and ovarian cancers. Genetic testing can help identify high-risk individuals. Those with a strong family history may opt for enhanced screening or preventive surgeries. Consulting with a genetic counsellor is recommended to understand future breast cancer risks.
8. Breast Cancer and Lifestyle Choices
Q: How do lifestyle choices affect breast cancer risk?
A: Lifestyle factors like a healthy diet, regular exercise, limiting alcohol, avoiding smoking, and maintaining a healthy weight can reduce breast cancer risk. Studies show that even moderate lifestyle changes can have a significant impact on reducing risk.
9. Treatment Options for Breast Cancer
Q: What are the common treatments for breast cancer?
A: Treatments depend on the type and stage of breast cancer and may include surgery, chemotherapy, radiation, targeted therapies, and hormone therapy. Personalized treatment plans ensure the best approach for each patient, helping to maximize survival rates.
10. The Importance of Support During Breast Cancer
Q: Why is support crucial for breast cancer patients?
A: Emotional and psychological support can make a significant difference for patients during and after treatment. Support groups, counseling, and family support help manage the emotional challenges of cancer, improving quality of life and recovery.
11. What is a Mammogram?
Q: What is a mammogram and why is it important?
A: A mammogram is a low-dose X-ray used to detect early signs of breast cancer, often before symptoms appear. Regular mammograms help catch cancer early when it’s more treatable. Women over 40 should have mammograms annually or as recommended by their doctor.
12. How Does Breast Cancer Spread?
Q: How does breast cancer spread in the body?
A: Breast cancer can spread when cells break away from the tumor and enter the lymphatic system or bloodstream. It can then spread to other parts of the body, such as the bones, liver, or lungs. Early diagnosis helps prevent the spread of cancer.
13. What is Triple-Negative Breast Cancer?
Q: What is triple-negative breast cancer?
A: Triple-negative breast cancer is an aggressive form of cancer that lacks estrogen, progesterone, and HER2 receptors. It doesn’t respond to hormonal therapies and requires other treatment methods like chemotherapy and Immunotherapy. It is more common in younger women and those with BRCA mutations.
14. Breast Cancer Myths and Facts
Q: What are some common myths about breast cancer?
A: Myth: Only women with a family history of breast cancer are at risk. Fact: Most women who get breast cancer have no family history. Myth: Wearing underwire bras or using antiperspirants causes breast cancer. Fact: There is no scientific evidence to support this.
15. Hormone Replacement Therapy and Breast Cancer
Q: How does hormone replacement therapy (HRT) affect breast cancer risk?
A: Long-term use of hormone replacement therapy (HRT), particularly combined estrogen-progestin therapy, has been linked to an increased risk of breast cancer. Women considering HRT should discuss the benefits and risks with their doctor.
16. Breast Cancer in Younger Women
Q: Can younger women develop breast cancer?
A: Yes, while breast cancer is more common in women over 50, younger women can also be affected. Genetic factors, lifestyle, and family history can increase risk. It’s important for young women to be aware of their bodies and seek medical advice if they notice unusual changes.
17. What is Metastatic Breast Cancer?
Q: What is metastatic breast cancer?
A: Metastatic breast cancer, also known as stage 4 breast cancer, occurs when cancer spreads beyond the breast to other parts of the body, like bones, liver, or lungs. Although it is not curable, treatments can help manage the disease and improve quality of life.
18. Breast Cancer and Pregnancy
Q: Can breast cancer affect pregnant women?
A: Yes, breast cancer can occur during pregnancy, though it’s rare. Diagnosis can be challenging as breasts naturally change during pregnancy. Treatment options depend on the stage of pregnancy and cancer but can be planned to protect both the mother and baby.
19. What Are the Types of Breast Cancer?
Q: What are the different types of breast cancer?
A: The two main types are invasive ductal carcinoma (IDC), which begins in the milk ducts, and invasive lobular carcinoma (ILC), which starts in the lobules. Other types include inflammatory breast cancer and ductal carcinoma in situ (DCIS), a non-invasive form. Breast cancer is further classified into subtypes based on hormone receptor status (estrogen, progesterone, HER2 receptors).
20. How Can Breast Cancer Be Prevented?
Q: Can breast cancer be prevented?
A: While breast cancer can’t always be prevented, reducing risk factors like maintaining a healthy weight, staying active, limiting alcohol, and avoiding smoking can lower the risk. For high-risk individuals, genetic testing and preventive treatments may also be considered.
10 questions focused on breast removal (mastectomy) and breast reconstruction through plastic surgery:
1. What is a Mastectomy?
Q: What is a mastectomy and why is it done?
A: A mastectomy is the surgical removal of one or both breasts, usually to treat or prevent breast cancer. It’s often recommended when the cancer is widespread or as a preventive measure for high-risk individuals.
2. Who is a Candidate for Breast Reconstruction?
Q: Who can undergo breast reconstruction after a mastectomy?
A: Most women who undergo mastectomy are eligible for breast reconstruction. Factors include overall health, cancer stage, and personal preference. Your surgeon will guide you through the options.
3. What Are the Types of Breast Reconstruction?
Q: What are the different types of breast reconstruction surgeries?
A: Reconstruction can involve implants (silicone or saline) or autologous tissue (using your own tissue from other parts of the body). The choice depends on individual factors like body type and cancer treatment.
4. When Can Breast Reconstruction Be Done?
Q: When can breast reconstruction be performed after mastectomy?
A: Breast reconstruction can be done either immediately during the mastectomy or delayed, depending on your medical condition and preference. Sometimes radiation or chemotherapy can delay reconstruction.
5. What Are the Risks of Breast Reconstruction?
Q: What are the risks and complications associated with breast reconstruction?
A: Risks include infection, implant rupture, changes in sensation, and scarring. Your surgeon will discuss potential risks based on your health and type of reconstruction.
6. How Long is the Recovery After Reconstruction?
Q: How long does recovery take after breast reconstruction surgery?
A: Recovery can take several weeks to months, depending on the type of surgery. Most women can return to normal activities within 4 to 6 weeks, but full recovery varies for each person.
7. Can Breast Reconstruction Restore Normal Appearance?
Q: Can breast reconstruction fully restore the appearance of natural breasts?
A: While breast reconstruction can create a natural-looking breast, it may not look or feel exactly the same as before. Advances in techniques can achieve a realistic appearance, but sensation may be different.
8. Will I Need Multiple Surgeries for Reconstruction?
Q: Will I need more than one surgery for breast reconstruction?
A: Yes at times, breast reconstruction involves multiple procedures over time. Additional surgeries may be needed to refine the shape, improve symmetry, or adjust implants.
9. What is Nipple Reconstruction?
Q: Can nipples be reconstructed after mastectomy?
A: Yes, nipple reconstruction is an option and can be done using tissue from the breast or other areas of the body. Nipple tattooing is another technique to create the appearance of a natural nipple.
10. How Does Radiation Affect Breast Reconstruction?
Q: Can I have breast reconstruction if I need radiation therapy?
A: Yes, but radiation can affect the timing and type of reconstruction. Radiation can damage reconstructed tissue, so some women opt for delayed reconstruction after completing their radiation therapy.



